Progress in sanitation and public health is still ongoing: the path towards the epidemiological transition
The sanitary state of a country and its population, its access to medical care, the investment in health that should naturally follow on, often reflect the level of development of that country.
The number of children dying at a young age, the epidemics which have not been eradicated, the alarming death rates attributable to malnutrition, the diseases once thought to have been stemmed now reappearing in one placed or another across the globe, are as much clear indicators of social and economic development of a particular country or region.
In the Caribbean region, the situation regarding public health and sanitation presents multiple facets. This spatial mosaic where one finds rich and developed countries side by side with those suffering profound human misery inevitably afford very different sanitary profiles. However, one constant is everywhere in evidence, namely that infectious diseases are very much in decline demonstrating that the efforts in public policies of humanitarian organisations, or again supra-national agencies, have begun to bear fruit. However, any such claim should be nuanced.
Certain diseases are proper to the geographical zone, such as malaria or other tropical diseases such as ‘Chagas,' a form of American trypanosomiasis, belonging to the same family as sleeping sickness, transmitted by a blood-sucking bug. Elsewhere, HIV/AIDS has ravaged the population ranks of countries in the Caribbean, where It continues to cut short the life expectancy of its populations by several years.
Public health and sanitation are as varied as the levels of development of Caribbean countries, but detailed analysis of the principal causes of mortality clearly reveals sub-groups of countries more affected than others by such and such a disease. The epidemiological transitions are underway. Access to care and spending on health supports these initial observations. HIV/AIDS is today a major cause of death in the Caribbean, even its occurrence geographically does not necessarily reflect economic indicators of development.
1. What does one die from in the Caribbean?
Sign of the times, of society's evolution, in the Caribbean more than any other cause, one dies from non-infection diseases, and particularly cardiovascular related illnesses. Life style, a richer diet, a more sedentary existence encourage the development of pathologies which are not solely the reserve of developed nations.
The mortality rate attributable to cardiovascular diseases attains an average of 222 deaths per 100 000 inhabitants in the Caribbean. The difference with countries from the northern hemisphere is slight, France reaching a rate of 257.5 deaths, and the United States, 317 deaths.1 In St. Kitts & Nevis, Antigua or even Barbados, regional record levels are attained, with more than 300 deaths each year per census count of 100 000 inhabitants. St. Kitts registers an even higher rate than neighbouring USA, with 388 deaths. In contrast, Guatemala and Mexico record rates well below the Caribbean average, with respectively 79.5 and 103 deaths.
Cancers represent the second most common cause of death in the region with a rate of around 94 deaths each year per 100 000 inhabitants. The highest totals are found in Grenada, Barbados, and Cuba where the number of deaths varies between 156 and 178 per annum. By comparison, in France the figure reaches 238.3 and 192 in the United States. The Caribbean thus appears relatively spared from this type of illness. Countries like El Salvador, Guatemala, Nicaragua or even Haiti, only register 50 or 60 deaths each year.
Degenerative or chronic illnesses are new to the region and testify to the completion of the epidemiological transition within most Caribbean countries. By the latter, one means that it is no longer the infectious diseases that cause the highest number of deaths but those non-infectious illnesses reflecting the improvements in sanitary and social conditions. Most significantly, the latter include access to drinking water, or improvements to sewage systems, but very unequally between different states. Much remains to be done for countries like Haiti if they are access an acceptable level of sanitation, and this first requires a general improvement in hygiene, access to drinking water, health care as well as self-sufficiency in food.
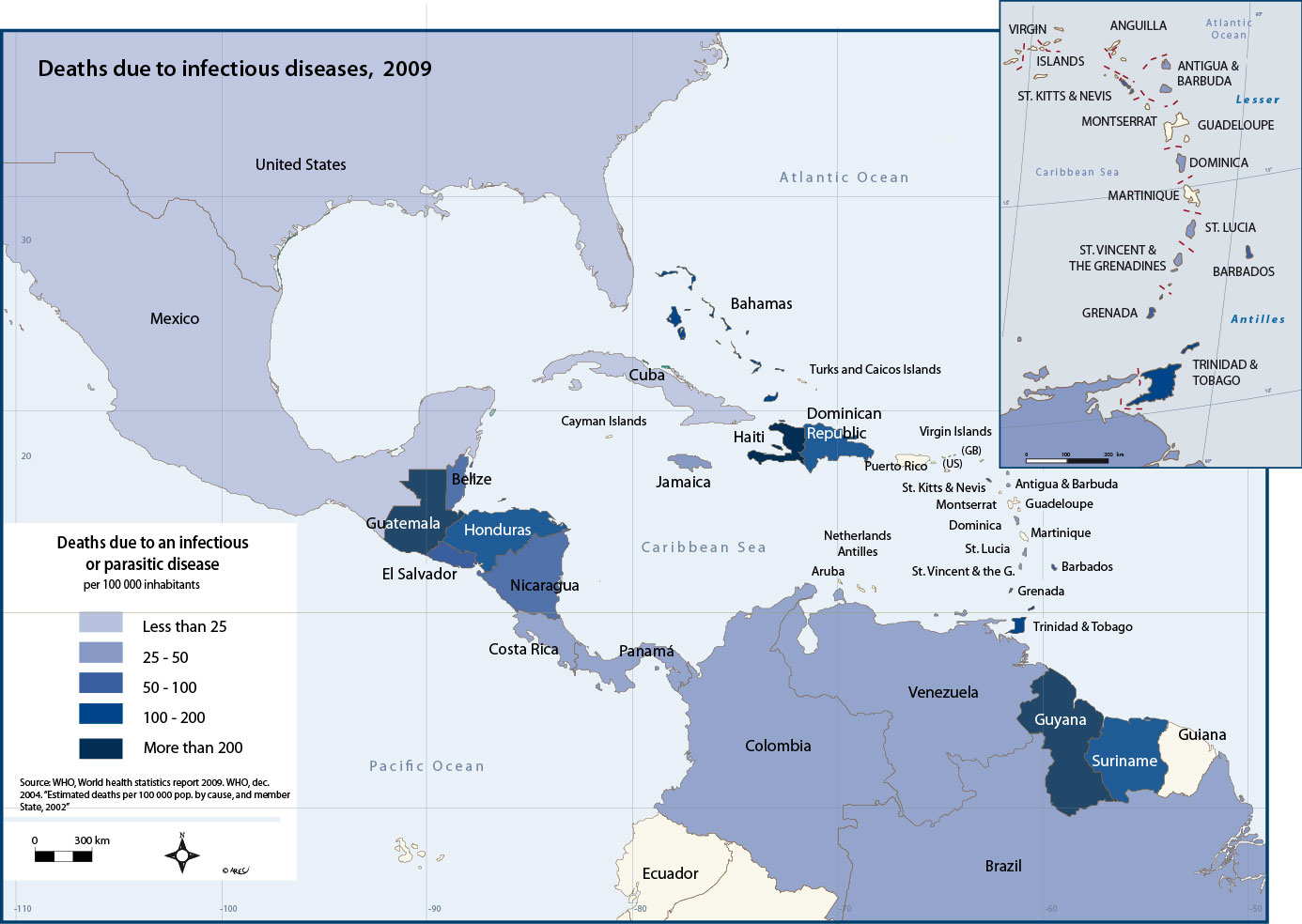
Deaths caused by infectious diseases (tuberculosis, diarrhoea, meningitis, respiratory failure) still occur in the Caribbean, but proportionately less so than in the past. The most affected countries include Haiti (102.9 deaths per 100 000 inhabitants), St. Kitts and Nevis (65), Cuba (59), and Grenada (57), the regional average being around 32 deaths per annum. At the other end of the scale, Costa Rica or the Bahamas register less than 15 deaths per annum per 100 000 inhabitants. The number of deaths from infectious diseases remains much lower than that for degenerative or chronic illnesses.
A country's level of development is one of the key factors explaining these rates, which in the case of Haiti for example are particularly bad. In contrast, infant mortality remains discriminatory in the Caribbean. In some countries, the rate often exceeds 25‰. According to the WHO, the campaign against high infants starts with improvements in perinatal surveillance. 37% of deaths of infants less than 5 years old occur in the first year of life, and mainly in the first week.
Progress has been achieved, particularly in improved vaccination cover, and in access to treatment and prevention, but the deaths of young mothers and young children still remains high. Mediocre sanitary conditions together with inadequate access to care and medical follow-up explain why the number of deaths is so closely linked to poor perinatal surveillance. Once again Haiti, but also Belize, Guyana, Honduras, or the Dominican Republic record 40 to 60 deaths each year. The latter appears high when compared to the figures for France (2.8) or the United States (5.5).
It is also in these same countries that today one still finds deaths caused by malnutrition. Agreed, the rates remain very low in all these states, less than 20 per 100 000 inhabitants, but one exception stands out: Haiti where the number of annual deaths reaches 62 per census count of 100 000 inhabitants. Conversely, Cuba or Costa Rica have less than one death per 100 000 inhabitants, i.e. lower than the figure for France (4.5).
Comparisons for the number of deaths due to degenerative and infectious diseases
To this list of current diseases, still present in many areas of the world, should be added those particularly associated with tropical environments.
Tropical diseases, whilst having been generally and efficiently eradicated, are still present in most countries of South America and the Isthmus, like ‘Chagas' particularly virulent in Brazil. One also finds a small number of deaths due to diseases like tuberculosis, diarrhoea, meningitis, or hepatitis B, but again only in a few countries, mainly Haiti, Guyana, Guatemala, Suriname, or the Dominican Republic.
Lastly, it should be noted that the main causes of recorded deaths in the Caribbean region are little different from those found in Europe or North America. There is one, however, that ignores national boundaries, and in its train sometimes ravages whole cohorts of a population, often the young: namely, HIV/AIDS.
2. AIDS also represents a veritable scourge in the Caribbean
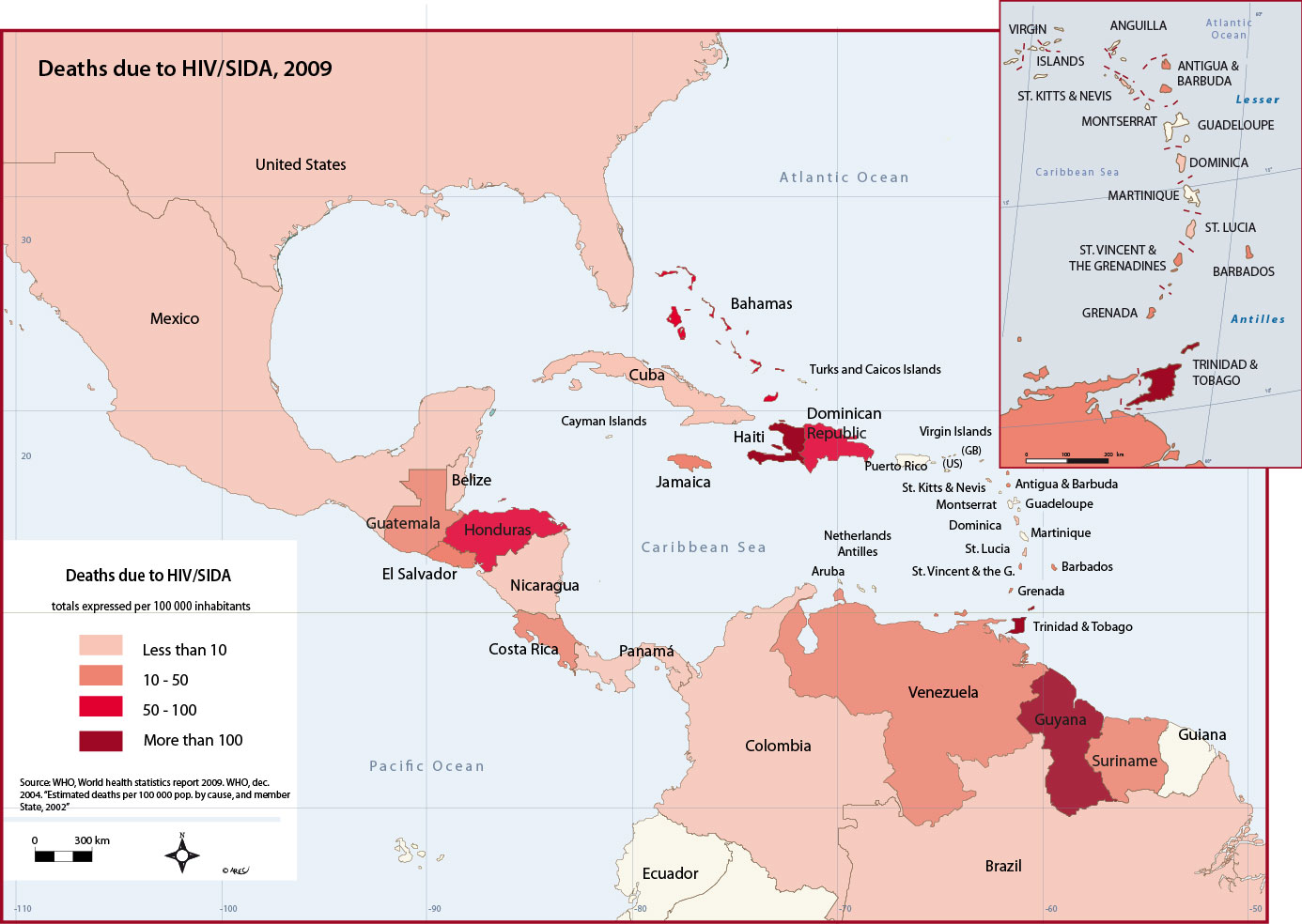
Despite the development of antiretroviral therapies, HIV has ravaged the populations of certain states in the Caribbean. It is particularly present in those states with poor conditions of sanitation and generally weak levels of social and economic development, but equally it is found in states that ‘a priori' one would have thought spared.
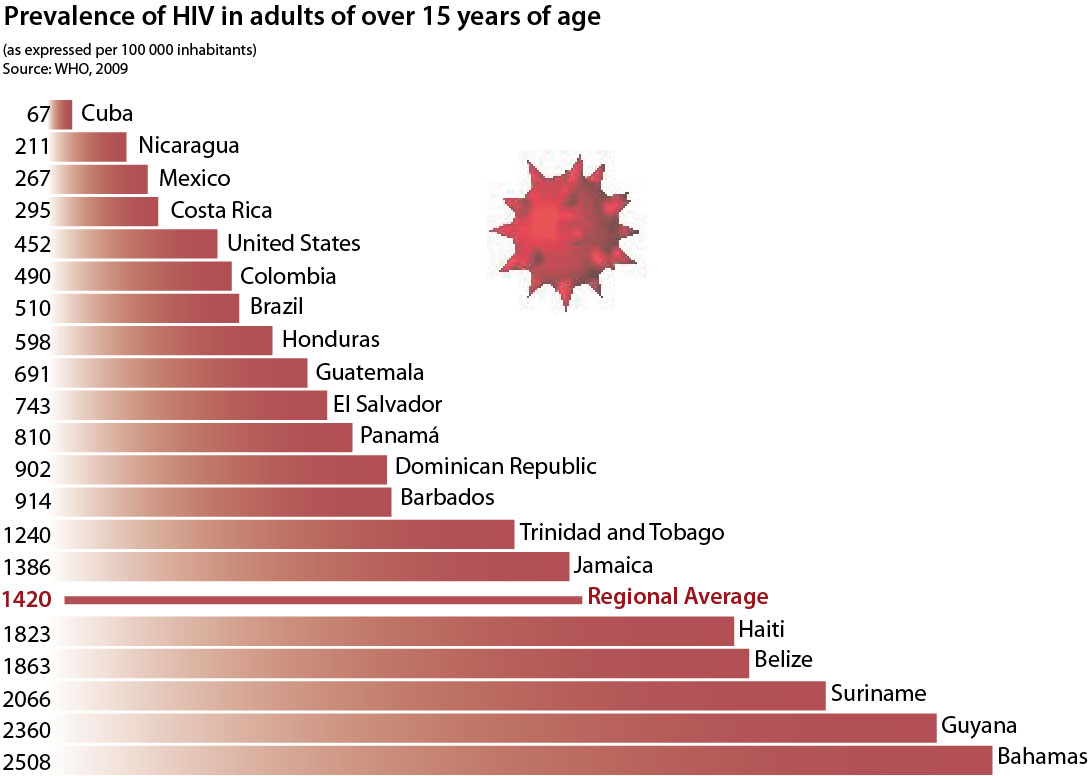
A few statistics help to substantiate this statement: the countries where the number of deaths per 100 000 inhabitants is the highest in decreasing is Haiti, Guyana, Trinidad and Tobago, Dominican Republic, and the Bahamas. In these states, the number of deaths rises above a maximum of 95, and can attain more than 300, as in the case of Haiti. By way of comparison, the number of deaths in France is of the order of 1.5 per 100 000 inhabitants. Within the above noted Caribbean group, the Bahamas appear as the “gate-crasher” in respect of their (advanced) level of development. In effect, the high rates found across these islands are explained by the presence of numerous expatriated Americans, and carriers of AIDS.
Looking at the statistics relating to the regional prevalence of HIV, one finds that in Central and South America the cohort of live individuals with AIDS is half as important as that in the rest of the world (0.5% of people between the ages of 15 and 49). However, at the scale of just the Caribbean region, the rate reaches 1.6%, i.e. significantly higher than the world average. The impact on mortality is far from negligible, given that the most heavily affected countries lose on average 5 years in life expectancy. As such, states like the Bahamas display very high death rates (9.2‰), explained by the incidence of AIDS and its impact on these islands. This epidemic also reveals a distinction between the sexes. It is essentially a masculine phenomenon in the Dominican Republic, Barbados, Suriname, or Belize, but feminine in Haiti, Honduras, or again Guyana, and does not show any significant distinction in the other states within the strongly affected HIV zone.
How does one explain such a negative picture across the Caribbean? Against a backdrop of inadequate information and health education, the reason also lies in the simple lack of access to antiretroviral therapies. In countries like Haiti or the Dominican Republic, where the prevalence is high, only 20% of those sick with the disease have access to this form of therapy.
Graph 1: Prevalence of HIV/AIDS in adults of over 15 years of age in the Caribbean (2007)
'Prevalence' measures the state of health of a population at a given date. It is calculated by relating the number of illnesses at that point in time to the total population (previously or recedntly diagnosed).
HIV/AIDS in the Caribbean
3. Contrasting situations in the Caribbean in the face of shortages of doctors and health workers
Sanitary conditions affecting populations can also be measured by reference to the availability of doctors and health workers.
Situations are very contrasted across the Caribbean. The world average as established by the WHO makes reference to 13 doctors per 10 000 inhabitants. The Bahamas, Belize, Colombia, Costa Rica, Brazil, El Salvador, Panama, Grenada, St. Kitts and Nevis are either on or around this average. If one considers those ‘medium-income' countries with qualified staff as defined par the WHO, the average come out at 22 doctors per 10 000 inhabitants. Only three countries either attain or approach near to this score: Mexico (20), Dominican Republic, and Venezuela (19). Otherwise, attaining the ratio of 27 doctors per 10 000 which defines the highest category, are only Cuba (59), and St. Lucia (52). By comparison, France has 34 doctors per 10 000 inhabitants, and the United States, 26.
All other countries in the Caribbean are below the world average, the lowest being Antigua & Barbuda with only 2 doctors per 10 000 inhabitants, which even Haiti surpasses with a score of 3.
The situations thus appear very contrasted and explain in part the poor rankings of many states in the Caribbean that suffer infectious diseases, as well as the large number of deaths at a young age because of the lack of perinatal surveillance.
Suriname, Honduras, Guyana, or again Dominica have between 5 and 6 doctors per 10 000 inhabitants. That is less than half the world average. It is these same countries that register the highest rates of morbidity within the Caribbean, Haiti excepted.
Medical personnel in the Caribbean in 2009
Turning to health workers, the variations are once again very marked. The WHO estimates that globally there are on average 28 nurses and midwives per 10 000 inhabitants. In the Caribbean region, the average is around 26. In relatives' terms, this appears to be acceptable when compared to the predicted figure for countries lying within that particular income range. As such, the Caribbean lies largely above the category of countries with ‘low average income,' where the average number of health workers is around 15 per 10 000. Similarly, the region compares relatively favourably to averages recorded in other parts of the world. With its average of 26 health workers per 10 000 inhabitants, the Caribbean is close to the European average of 32, and well above that given for the Region of the Americas, namely 19.
Such an average nevertheless conceals very high variations and not least some exceptional situations. Disparities between countries across the zone, with at one end of the scale Cuba and St. Kitts & Nevis, where the average number of health workers exceeds 45 per 10 000 inhabitants (the maximum recorded is Cuba with 74). At the other end, Haiti, Colombia, and El Salvador have on average less than 10 health workers, with Haiti lying at the bottom of the table with just one health worker per 10 000 inhabitants.
On more close examination of the WHO data, it appears that the rates of morbidity can be directly linked to the availability or otherwise of medical personnel. However, this is not the only fact to emerge. More startling is that in the Caribbean region some countries have less health workers (whether nurses or midwives) than doctors: it is the case in Haiti, El Salvador, Costa Rica, Colombia, Mexico, St. Lucia, and Venezuela. In reality, the problem is even worse than it appears. What concern the WHO is not so much that doctors appear to outnumber nurses or midwives but that for several years there has been a real shortage of health workforce, all categories subsumed. Africa presents the greatest disparities between total population and medical support needs, but the Caribbean is far from exempted. This situation can no longer be viewed as a mere preoccupation; it has become a priority at the heart of WHO policy statements, the issue having been the subject of the organisation's 2006 annual report.
The reasons for this shortage are many and varied: the ageing of the existing personnel, the social and economic attraction of developed countries leading to a “brain drain,” the increased number of personnel staff afflicted by illness and death. In many remote and unattractive geographical areas, the doctor fulfils all the roles of nurse, midwife, and specialist. Such situations will not be without consequence for the sanitary conditions of the populations in question.
The reverse of this situation is found in those countries of the Caribbean where medical personnel represent more than twice the total number of doctors. It is a situation still found in countries like France and the United States, also now beginning to face a growing shortage of health workers. Some Caribbean countries stand out in terms of health workers like Cuba or the Bahamas, Dominica... In turn, the generous availability of such personnel helps explain the high rates of life expectancy, as in Cuba. In just two countries, a close balance exists between doctors and paramedical staff: Belize and the Dominican Republic. But regionally the limits have now been reached. If very soon, measures are not taken to reduce the flight of personnel to more attractive jobs in neighbouring countries, or to nearby USA, or towards Europe, the Caribbean in the more or less long term will face the difficulties now confronting Southeast Asia or Africa in matters of health care. The shortage of personnel is aggravating sanitary situations that are already fragile. For countries like the Dominican Republic or Belize, one can only be fearful of a rapid deterioration of health care systems, this despite the efforts undertaken to combat infectious pathologies, and to provide improved perinatal surveillance. Without adequate personnel, there can be no follow-up, no efficient taking into care of the sick, and the risk of mortality rates rising once again.
The level of development, the economic situation, the disposable wealth, the efficiency of the education system are all clearly major factors affecting improvements in sanitary conditions and the fight against the rate of morbidity. They impact directly on the sanitary levels of countries and populations, and conversely this same measure plays a fundamental role in the level of development of the state.
4. Lower rates of health expenditures as compared to the world average
The state of sanitation is often used to characterise the economic level of a country. Its direct counterpart in terms of health is the total expenditure of a state devoted to health care.
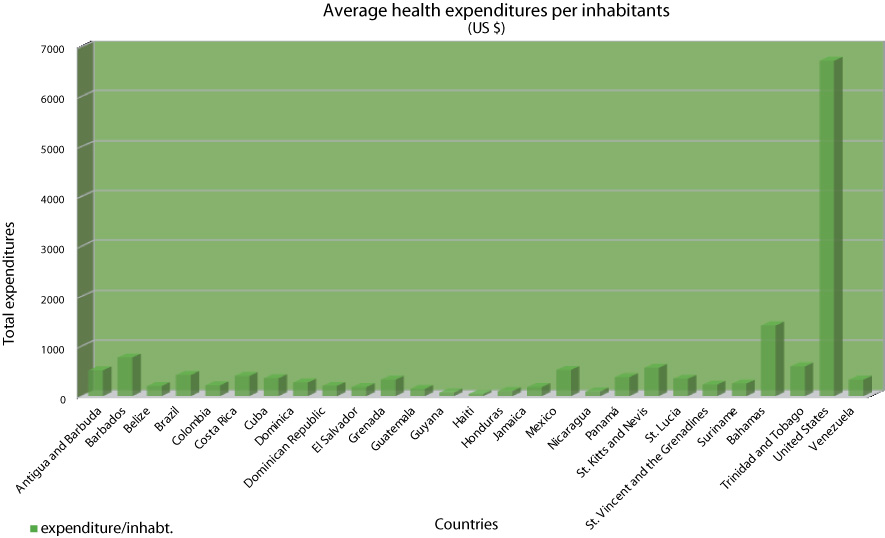
At the global scale, health expenditure in 2006 (according to the WHO) rose to some 8.7% of GDP, which corresponds to around 716 USD on average per head of population, i.e. less than 2 USD per day and per inhabitant, and a state contribution of over 50% of expenditure in this domain. Very important variations are evident between parts of the world. In the Caribbean, the total health expenditure per inhabitant is nearly 440 USD, i.e. half the global average. This figure places the whole region below the world average.
Haiti spends on average 42 USD per inhabitant on health care. In contrast to this extreme example, the Bahamas or Barbados record much higher levels per capita of expenditure, above the world average. The diversity of sanitary situations observed in the region all find expression in the degrees of investment made by the different states in their health sectors. On average, health expenditure represents 6.4% of GDP in the region's countries, and these states each contributed up to 56% of the cost of their own health system. This relatively good contribution however conceals significant variations: the government of Cuba finances more than 90% of the national health system, whilst the Dominican Republic contributes only 37% The remaining 63% is made up by private contributions, the major part of which borne by the patient. In Haiti, for example, the state contributes up to 68% of the total costs, with the remaining 32% coming from private sources (around 90% which from the patient). Given the low standards of living of the Haitian population, it is easy to understand the poor results in terms or health care provided. How does one protect one's health when already suffering from too little to eat? The more the country is economically deprived, the greater the cost for the individual health has a price, which itself accentuates disparities, which themselves in turn directly influence the country's level of development.
In systems where the state no longer has the capacity economically to engage further, the shortfall has to be met by the private sector. This is the case in Haiti, where 66% of funding come from external sources. The risks of breakdown of the system are high in the case of disengagement by the funders.
Graph 2: Average health expenditure per inhabitant (USD)
Graph 3: % health expenditure as a proportion of national GDP
Even if the epidemiological transition is complete, if sanitary conditions have improved, and pathologies increasingly compare to those of the countries of the North, much remains to be done in matters of health. The countries of the Caribbean are on the right road but as their situations see more rapid improvement, they risk being confronted by thornier problems of shortages in qualified personnel. Measures to encourage new recruitment need to be put in place in the near future in order to preserve an efficient level of health workers across the region, so as to guarantee access to care for everyone.
In respect of diseases, the fight against infectious pathologies is producing results, even though further actions remain to be taken, particularly regarding follow-up care for babies and young mothers. Lastly, AIDS remains a scourge, and kills because of both lack of information and means. Vigilance is still the order of the day.
top
|
  |